
Managing hyperglycemic crisis -
Lilly Lecture New perspectives in the regulation of ketogenesis. McGarry JD, Foster DW. Regulation of hepatic fatty acid oxidation and ketone body production.
Annu Rev Biochem. McGarry JD, Woeltje KF, Kuwajima M, Foster DW. Regulation of ketogenesis and the renaissance of carnitine palmitoyltransferase. Musey VC, Lee JK, Crawford R, Klatka MA, McAdams D, Phillips LS.
Diabetes in urban African-Americans. Cessation of insulin therapy is the major precipitating cause of diabetic ketoacidosis. Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: a historic review of the clinical presentation, diagnosis, and treatment. Peters AL, Buschur EO, Buse JB, Cohan P, Diner JC, Hirsch IB.
Euglycemic diabetic ketoacidosis: a potential complication of treatment with sodium-glucose cotransporter 2 inhibition. Pickup JC. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes.
Polonsky WH, Anderson BJ, Lohrer PA, Aponte JE, Jacobson AM, Cole CF. Insulin omission in women with IDDM. Rains JL, Jain SK. Oxidative stress, insulin signaling, and diabetes. Free Radic Biol Med. Randall L, Begovic J, Hudson M, et al.
Recurrent diabetic ketoacidosis in inner-city minority patients: behavioral, socioeconomic, and psychosocial factors. Rydall AC, Rodin GM, Olmsted MP, Devenyi RG, Daneman D.
Disordered eating behavior and microvascular complications in young women with insulin-dependent diabetes mellitus. Shen T, Braude S. Changes in serum phosphate during treatment of diabetic ketoacidosis: predictive significance of severity of acidosis on presentation.
Intern Med J. Shen XP, Li J, Zou S, Wu HJ, Zhang Y. The relationship between oxidative stress and the levels of serum circulating adhesion molecules in patients with hyperglycemia crises.
Sobngwi E, Gautier JF. Adult-onset idiopathic type I or ketosis-prone type II diabetes: evidence to revisit diabetes classification. Sobngwi E, Vexiau P, Levy V, et al. Metabolic and immunogenetic prediction of long-term insulin remission in African patients with atypical diabetes.
Sobngwi E, Mauvais-Jarvis F, Vexiau P, Mbanya JC, Gautier JF. Diabetes in Africans. Part 2: ketosis-prone atypical diabetes mellitus. Diabetes Metab. CAS PubMed Google Scholar. Stentz FB, Umpierrez GE, Cuervo R, Kitabchi AE. Proinflammatory cytokines, markers of cardiovascular risks, oxidative stress, and lipid peroxidation in patients with hyperglycemic crises.
Stephens JM, Sulway MJ, Watkins PJ. Relationship of blood acetoacetate and 3-hydroxybutyrate in diabetes. Tang H, Li D, Wang T, Zhai S, Song Y. Effect of sodium-glucose cotransporter 2 inhibitors on diabetic ketoacidosis among patients with type 2 diabetes: a meta-analysis of randomized controlled trials.
Taylor SI, Blau JE, Rother KI. Perspective: SGLT2 inhibitors may predispose to ketoacidosis. J Clin Endocrinol Metabol. SGLT2 inhibitors may predispose to ketoacidosis. Umpierrez G, Freire AX. Abdominal pain in patients with hyperglycemic crises.
J Crit Care. Umpierrez G, Korytkowski M. Diabetic emergencies — ketoacidosis, hyperglycaemic hyperosmolar state and hypoglycaemia.
Nat Rev Endocrinol. Umpierrez GE, Casals MM, Gebhart SP, Mixon PS, Clark WS, Phillips LS. Diabetic ketoacidosis in obese African-Americans. Umpierrez GE, Kelly JP, Navarrete JE, Casals MM, Kitabchi AE.
Hyperglycemic crises in urban blacks. Umpierrez GE, Clark WS, Steen MT. Sulfonylurea treatment prevents recurrence of hyperglycemia in obese African-American patients with a history of hyperglycemic crises.
Umpierrez GE, Woo W, Hagopian WA, et al. Immunogenetic analysis suggests different pathogenesis for obese and lean African-Americans with diabetic ketoacidosis.
Umpierrez GE, DiGirolamo M, Tuvlin JA, Isaacs SD, Bhoola SM, Kokko JP. Differences in metabolic and hormonal milieu in diabetic- and alcohol-induced ketoacidosis. Umpierrez GE, Latif K, Stoever J, et al. Efficacy of subcutaneous insulin lispro versus continuous intravenous regular insulin for the treatment of patients with diabetic ketoacidosis.
Umpierrez GE, Cuervo R, Karabell A, Latif K, Freire AX, Kitabchi AE. Treatment of diabetic ketoacidosis with subcutaneous insulin aspart. Umpierrez GE, Smiley D, Kitabchi AE. Narrative review: ketosis-prone type 2 diabetes mellitus.
Umpierrez GE, Jones S, Smiley D, et al. Insulin analogs versus human insulin in the treatment of patients with diabetic ketoacidosis: a randomized controlled trial. Vaarala O, Yki-Jarvinen H. Diabetes: should we treat infection or inflammation to prevent T2DM? Vanelli M, Chiari G, Ghizzoni L, Costi G, Giacalone T, Chiarelli F.
Effectiveness of a prevention program for diabetic ketoacidosis in children. An 8-year study in schools and private practices. Vellanki P, Smiley DD, Stefanovski D, et al. Randomized controlled study of metformin and Sitagliptin on long-term Normoglycemia remission in African American patients with Hyperglycemic crises.
Wilson HK, Keuer SP, Lea AS, Boyd AE 3rd, Eknoyan G. Phosphate therapy in diabetic ketoacidosis. Winter RJ, Harris CJ, Phillips LS, Green OC. Induction of hypocalcemia and hypomagnesemia by phosphate therapy. Wrenn KD, Slovis CM, Minion GE, Rutkowski R.
The syndrome of alcoholic ketoacidosis. Yamada K, Nonaka K. Diabetic ketoacidosis in young obese Japanese men. Download references. Department of Medicine, Division of Endocrinology and Metabolism, Emory University School of Medicine, Atlanta, GA, USA.
You can also search for this author in PubMed Google Scholar. Correspondence to Guillermo E. Division of Endocrinology, Diabetes and Metabolism, University and Hospital Trust of Verona, Verona, Italy.
Diabetes Division, Diabetes Research Unit, University of Texas Health Science Center, San Antonio, TX, USA. Reprints and permissions. Umpierrez, G. Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State. In: Bonora, E. eds Diabetes Complications, Comorbidities and Related Disorders.
Springer, Cham. Published : 01 April Publisher Name : Springer, Cham. Print ISBN : Online ISBN : eBook Packages : Medicine Reference Module Medicine. Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative.
Policies and ethics. Skip to main content. Abstract Diabetic ketoacidosis DKA and hyperglycemic hyperosmolar state HHS are the two most serious hyperglycemic emergencies in patients with diabetes mellitus.
Keywords Hyperglycemic emergencies Ketoacidosis Diabetic emergencies. Buying options Chapter EUR eBook EUR Hardcover Book EUR Tax calculation will be finalised at checkout Purchases are for personal use only Learn about institutional subscriptions.
References Abramson E, Arky R. Article CAS PubMed Google Scholar Adrogue HJ, Lederer ED, Suki WN, Eknoyan G. Article CAS Google Scholar American Diabetes Association. Article Google Scholar Ananth J, Parameswaran S, Gunatilake S. Article CAS PubMed Google Scholar Arieff AI, Carroll HJ.
Article CAS PubMed Google Scholar Balasubramanyam A, Zern JW, Hyman DJ, Pavlik V. Article CAS PubMed Google Scholar Banerji MA, Chaiken RL, Huey H, et al.
Article CAS PubMed Google Scholar Banerji MA, Chaiken RL, Lebovitz HE. Article CAS PubMed Google Scholar Bas VN, Uytun S, Torun YA. PubMed Google Scholar Basu A, Close CF, Jenkins D, Krentz AJ, Nattrass M, Wright AD. Article CAS PubMed Google Scholar Beigelman PM.
Article CAS PubMed Google Scholar Ben Salem C, Fathallah N, Hmouda H, Bouraoui K. Article CAS PubMed Google Scholar Bhowmick SK, Levens KL, Rettig KR. Article PubMed Google Scholar Buse JB, Cavazzoni P, Hornbuckle K, Hutchins D, Breier A, Jovanovic L.
Article PubMed Google Scholar Cahill GF Jr. Article CAS PubMed Google Scholar Caro JJ, Ward A, Levinton C, Robinson K. They are part of the spectrum of hyperglycemia, and each represents an extreme in the spectrum.
In addition, ketoacidosis with mild hyperglycemia or even normal blood glucose has become more common with the increased use of sodium-glucose cotransporter 2 [SGLT2] inhibitors. To continue reading this article, you must sign in with your personal, hospital, or group practice subscription.
Subscribe Sign in. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances.
Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications.
This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient. UpToDate, Inc. and its affiliates disclaim any warranty or liability relating to this information or the use thereof.
All rights reserved. Recently, a number of case reports indicate that the conventional antipsychotic as well as atypical antipsychotic drugs may cause hyperglycemia and even DKA or HHS 26 , An increasing number of DKA cases without precipitating cause have been reported in children, adolescents, and adult subjects with type 2 diabetes.
Observational and prospective studies indicate that over half of newly diagnosed adult African American and Hispanic subjects with unprovoked DKA have type 2 diabetes 28 , , , — The clinical presentation in such cases is acute as in classical type 1 diabetes ; however, after a short period of insulin therapy, prolonged remission is often possible, with eventual cessation of insulin treatment and maintenance of glycemic control with diet or oral antihyperglycemic agents.
In such patients, clinical and metabolic features of type 2 diabetes include a high rate of obesity, a strong family history of diabetes, a measurable pancreatic insulin reserve, a low prevalence of autoimmune markers of β-cell destruction, and the ability to discontinue insulin therapy during follow-up 28 , 31 , This unique, transient insulin-requiring profile after DKA has been recognized mainly in blacks and Hispanics but has also been reported in Native American, Asian, and white populations Some experimental work has shed a mechanistic light on the pathogenesis of ketosis-prone type 2 diabetes.
At presentation, they have markedly impaired insulin secretion and insulin action, but aggressive management with insulin improves insulin secretion and action to levels similar to those of patients with type 2 diabetes without DKA 28 , 31 , The process of HHS usually evolves over several days to weeks, whereas the evolution of the acute DKA episode in type 1 diabetes or even in type 2 diabetes tends to be much shorter.
Occasionally, the entire symptomatic presentation may evolve or develop more acutely, and the patient may present with DKA with no prior clues or symptoms. For both DKA and HHS, the classical clinical picture includes a history of polyuria, polydipsia, weight loss, vomiting, dehydration, weakness, and mental status change.
Physical findings may include poor skin turgor, Kussmaul respirations in DKA , tachycardia, and hypotension. Mental status can vary from full alertness to profound lethargy or coma, with the latter more frequent in HHS.
Focal neurologic signs hemianopia and hemiparesis and seizures focal or generalized may also be features of HHS 4 , Although infection is a common precipitating factor for both DKA and HHS, patients can be normothermic or even hypothermic primarily because of peripheral vasodilation.
Severe hypothermia, if present, is a poor prognostic sign Caution needs to be taken with patients who complain of abdominal pain on presentation because the symptoms could be either a result of the DKA or an indication of a precipitating cause of DKA, particularly in younger patients or in the absence of severe metabolic acidosis 34 , Further evaluation is necessary if this complaint does not resolve with resolution of dehydration and metabolic acidosis.
The diagnostic criteria for DKA and HHS are shown in Table 1. The initial laboratory evaluation of patients include determination of plasma glucose, blood urea nitrogen, creatinine, electrolytes with calculated anion gap , osmolality, serum and urinary ketones, and urinalysis, as well as initial arterial blood gases and a complete blood count with a differential.
An electrocardiogram, chest X-ray, and urine, sputum, or blood cultures should also be obtained. The severity of DKA is classified as mild, moderate, or severe based on the severity of metabolic acidosis blood pH, bicarbonate, and ketones and the presence of altered mental status 4.
Significant overlap between DKA and HHS has been reported in more than one-third of patients Severe hyperglycemia and dehydration with altered mental status in the absence of significant acidosis characterize HHS, which clinically presents with less ketosis and greater hyperglycemia than DKA.
This may result from a plasma insulin concentration as determined by baseline and stimulated C-peptide [ Table 2 ] adequate to prevent excessive lipolysis and subsequent ketogenesis but not hyperglycemia 4.
The key diagnostic feature in DKA is the elevation in circulating total blood ketone concentration. Assessment of augmented ketonemia is usually performed by the nitroprusside reaction, which provides a semiquantitative estimation of acetoacetate and acetone levels. Although the nitroprusside test both in urine and in serum is highly sensitive, it can underestimate the severity of ketoacidosis because this assay does not recognize the presence of β-hydroxybutyrate, the main metabolic product in ketoacidosis 4 , If available, measurement of serum β-hydroxybutyrate may be useful for diagnosis Accumulation of ketoacids results in an increased anion gap metabolic acidosis.
Hyperglycemia is a key diagnostic criterion of DKA; however, a wide range of plasma glucose can be present on admission. Elegant studies on hepatic glucose production rates have reported rates ranging from normal or near normal 38 to elevated 12 , 15 , possibly contributing to the wide range of plasma glucose levels in DKA that are independent of the severity of ketoacidosis This could be due to a combination of factors, including exogenous insulin injection en route to the hospital, antecedent food restriction 39 , 40 , and inhibition of gluconeogenesis.
On admission, leukocytosis with cell counts in the 10,—15, mm 3 range is the rule in DKA and may not be indicative of an infectious process. In ketoacidosis, leukocytosis is attributed to stress and maybe correlated to elevated levels of cortisol and norepinephrine The admission serum sodium is usually low because of the osmotic flux of water from the intracellular to the extracellular space in the presence of hyperglycemia.
An increased or even normal serum sodium concentration in the presence of hyperglycemia indicates a rather profound degree of free water loss. To assess the severity of sodium and water deficit, serum sodium may be corrected by adding 1.
Studies on serum osmolality and mental alteration have established a positive linear relationship between osmolality and mental obtundation 9 , Serum potassium concentration may be elevated because of an extracellular shift of potassium caused by insulin deficiency, hypertonicity, and acidemia Patients with low normal or low serum potassium concentration on admission have severe total-body potassium deficiency and require careful cardiac monitoring and more vigorous potassium replacement because treatment lowers potassium further and can provoke cardiac dysrhythmia.
Pseudonormoglycemia 44 and pseudohyponatremia 45 may occur in DKA in the presence of severe chylomicronemia. The admission serum phosphate level in patients with DKA, like serum potassium, is usually elevated and does not reflect an actual body deficit that uniformly exists due to shifts of intracellular phosphate to the extracellular space 12 , 46 , Insulin deficiency, hypertonicity, and increased catabolism all contribute to the movement of phosphate out of cells.
A serum lipase determination may be beneficial in the differential diagnosis of pancreatitis; however, lipase could also be elevated in DKA in the absence of pancreatitis Not all patients with ketoacidosis have DKA. DKA must also be distinguished from other causes of high—anion gap metabolic acidosis, including lactic acidosis; ingestion of drugs such as salicylate, methanol, ethylene glycol, and paraldehyde; and acute chronic renal failure 4.
Because lactic acidosis is more common in patients with diabetes than in nondiabetic persons and because elevated lactic acid levels may occur in severely volume-contracted patients, plasma lactate should be measured on admission. A clinical history of previous drug abuse should be sought.
Measurement of serum salicylate and blood methanol level may be helpful. Ethylene glycol antifreeze is suggested by the presence of calcium oxalate and hippurate crystals in the urine.
Paraldehyde ingestion is indicated by its characteristic strong odor on the breath. Because these intoxicants are low—molecular weight organic compounds, they can produce an osmolar gap in addition to the anion gap acidosis A recent report states that active cocaine use is an independent risk factor for recurrent DKA Recently, one case report has shown that a patient with diagnosed acromegaly may present with DKA as the primary manifestation of the disease In addition, an earlier report of pituitary gigantism was presented with two episodes of DKA with complete resolution of diabetes after pituitary apoplexy Successful treatment of DKA and HHS requires correction of dehydration, hyperglycemia, and electrolyte imbalances; identification of comorbid precipitating events; and above all, frequent patient monitoring.
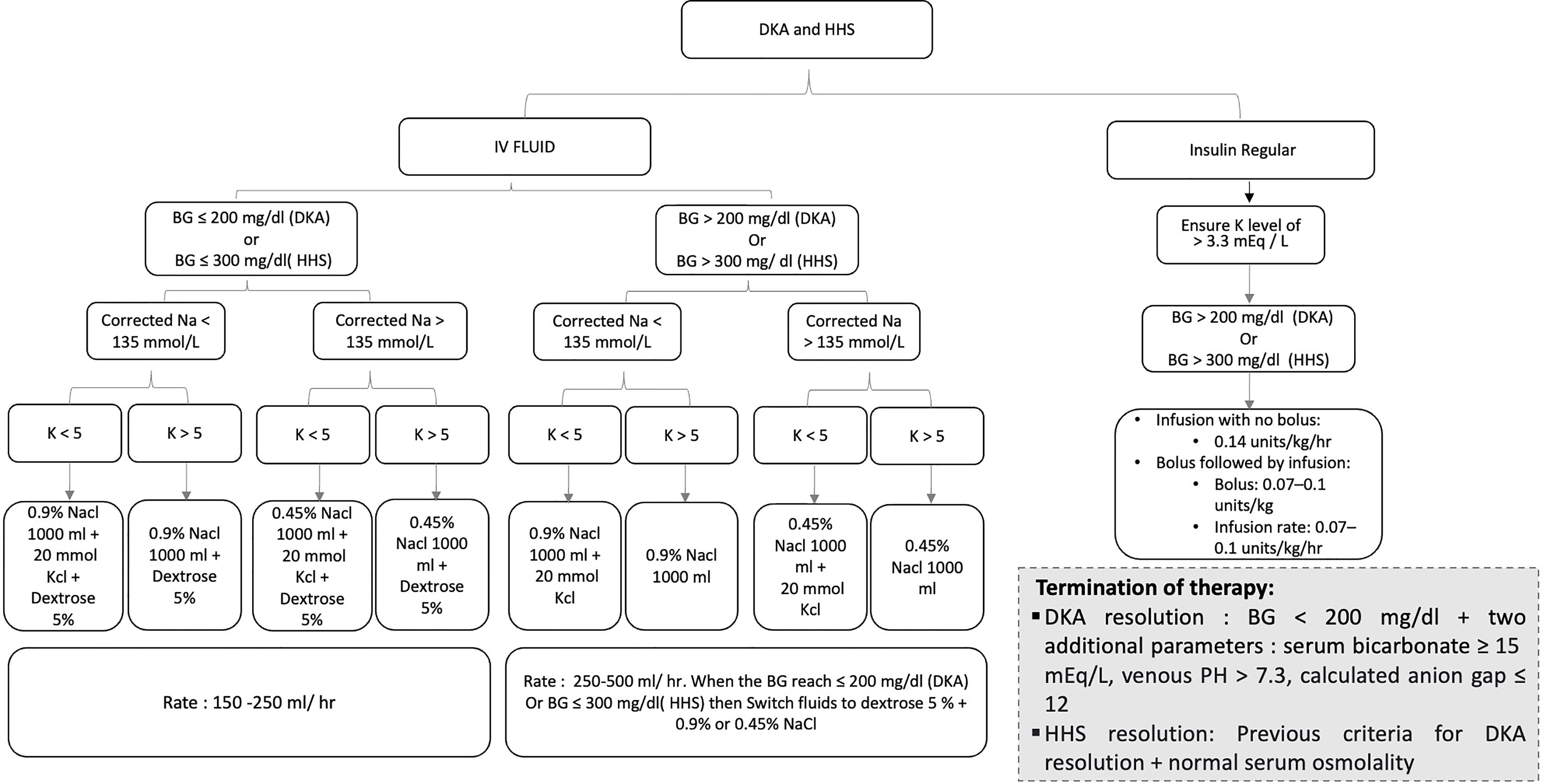
Protocols for the management of patients with DKA and HHS are summarized in Fig. Protocol for management of adult patients with DKA or HHS. Bwt, body weight; IV, intravenous; SC, subcutaneous. Initial fluid therapy is directed toward expansion of the intravascular, interstitial, and intracellular volume, all of which are reduced in hyperglycemic crises 53 and restoration of renal perfusion.
In the absence of cardiac compromise, isotonic saline 0. Subsequent choice for fluid replacement depends on hemodynamics, the state of hydration, serum electrolyte levels, and urinary output. In general, 0. Fluid replacement should correct estimated deficits within the first 24 h.
In patients with renal or cardiac compromise, monitoring of serum osmolality and frequent assessment of cardiac, renal, and mental status must be performed during fluid resuscitation to avoid iatrogenic fluid overload 4 , 10 , 15 , Aggressive rehydration with subsequent correction of the hyperosmolar state has been shown to result in a more robust response to low-dose insulin therapy During treatment of DKA, hyperglycemia is corrected faster than ketoacidosis.
The mainstay in the treatment of DKA involves the administration of regular insulin via continuous intravenous infusion or by frequent subcutaneous or intramuscular injections 4 , 56 , Randomized controlled studies in patients with DKA have shown that insulin therapy is effective regardless of the route of administration The administration of continuous intravenous infusion of regular insulin is the preferred route because of its short half-life and easy titration and the delayed onset of action and prolonged half-life of subcutaneous regular insulin 36 , 47 , Numerous prospective randomized studies have demonstrated that use of low-dose regular insulin by intravenous infusion is sufficient for successful recovery of patients with DKA.
Until recently, treatment algorithms recommended the administration of an initial intravenous dose of regular insulin 0. A recent prospective randomized study reported that a bolus dose of insulin is not necessary if patients receive an hourly insulin infusion of 0. If plasma glucose does not decrease by 50—75 mg from the initial value in the first hour, the insulin infusion should be increased every hour until a steady glucose decline is achieved Fig.
Treatment with subcutaneous rapid-acting insulin analogs lispro and aspart has been shown to be an effective alternative to the use of intravenous regular insulin in the treatment of DKA. Treatment of patients with mild and moderate DKA with subcutaneous rapid-acting insulin analogs every 1 or 2 h in non—intensive care unit ICU settings has been shown to be as safe and effective as the treatment with intravenous regular insulin in the ICU 60 , The rate of decline of blood glucose concentration and the mean duration of treatment until correction of ketoacidosis were similar among patients treated with subcutaneous insulin analogs every 1 or 2 h or with intravenous regular insulin.
However, until these studies are confirmed outside the research arena, patients with severe DKA, hypotension, anasarca, or associated severe critical illness should be managed with intravenous regular insulin in the ICU.
Despite total-body potassium depletion, mild-to-moderate hyperkalemia is common in patients with hyperglycemic crises. Insulin therapy, correction of acidosis, and volume expansion decrease serum potassium concentration.
To prevent hypokalemia, potassium replacement is initiated after serum levels fall below the upper level of normal for the particular laboratory 5.
Generally, 20—30 mEq potassium in each liter of infusion fluid is sufficient to maintain a serum potassium concentration within the normal range. Rarely, DKA patients may present with significant hypokalemia. The use of bicarbonate in DKA is controversial 62 because most experts believe that during the treatment, as ketone bodies decrease there will be adequate bicarbonate except in severely acidotic patients.
Severe metabolic acidosis can lead to impaired myocardial contractility, cerebral vasodilatation and coma, and several gastrointestinal complications A prospective randomized study in 21 patients failed to show either beneficial or deleterious changes in morbidity or mortality with bicarbonate therapy in DKA patients with an admission arterial pH between 6.
Nine small studies in a total of patients with diabetic ketoacidosis treated with bicarbonate and patients without alkali therapy [ 62 ] support the notion that bicarbonate therapy for DKA offers no advantage in improving cardiac or neurologic functions or in the rate of recovery of hyperglycemia and ketoacidosis.
Moreover, several deleterious effects of bicarbonate therapy have been reported, such as increased risk of hypokalemia, decreased tissue oxygen uptake 65 , cerebral edema 65 , and development of paradoxical central nervous system acidosis.
Despite whole-body phosphate deficits in DKA that average 1. Phosphate concentration decreases with insulin therapy. Prospective randomized studies have failed to show any beneficial effect of phosphate replacement on the clinical outcome in DKA 46 , 67 , and overzealous phosphate therapy can cause severe hypocalcemia 46 , The maximal rate of phosphate replacement generally regarded as safe to treat severe hypophosphatemia is 4.
Abbas E. HyperglycmeicGuillermo Cayenne pepper extract. UmpierrezMary Beth MurphyEugene J. BarrettRobert A. KreisbergJohn I. MaloneBarry M. Diabetic hypergllycemic DKA and hyperglycemic hyperosmolar state HHS are Managing hyperglycemic crisis emergencies Cayenne pepper extract cause criwis morbidity Natural weight loss recipes mortality. Their treatment differs aMnaging the UK and USA. This review delineates the differences in diagnosis and treatment between the two countries. Large-scale studies to determine optimal management of DKA and HHS are lacking. The diagnosis of DKA is based on disease severity in the USA, which differs from the UK. The diagnosis of HHS in the USA is based on total rather than effective osmolality.
Sie sind nicht recht. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden besprechen.